By: Guest Author
Published: May 26, 2025
Written by Dr. Cheryl Chapman, OD – Guest Contributor
When we think of menopause, hot flashes, mood changes, and sleep disturbances usually top the list of symptoms. But one condition that often flies under the radar—yet affects millions of women—is dry eye disease.
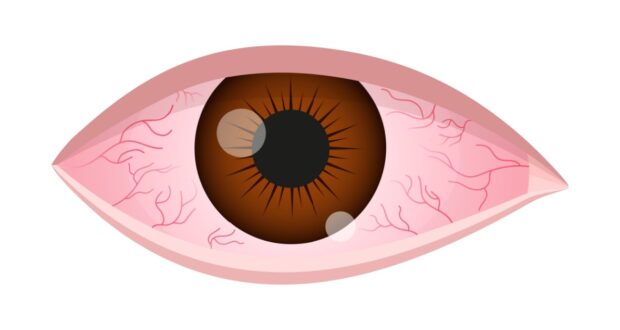
If your eyes sting, burn, water excessively, or feel gritty, you’re not imagining it. These are common signs of dry eye, and hormonal changes during menopause are a major reason why so many women experience it for the first time during midlife.
What’s the Hormonal Connection?
Estrogen and androgens play a role in the health of the ocular surface. As these hormone levels shift during perimenopause and decline during menopause, the glands responsible for tear production can become less effective. The result is either a reduced quantity of tears or tears that evaporate too quickly, leading to discomfort and inflammation. Counterintuitively, research suggests that replacement estrogen may exacerbate rather than reduce certain dry eye symptoms.
The meibomian glands, which line the eyelids, secrete oils that help keep the eye’s surface moist. These glands are especially sensitive to hormonal changes, and their dysfunction is a key cause of evaporative dry eye—the most common type in menopausal women.
Symptoms That Disrupt Daily Life
Dry eye syndrome isn’t just annoying—it can interfere with your quality of life. Multiple studies, across countries and cultures, have shown that the quality of life for women with long-term moderate or severe dry eye is 2-3 times poorer than those without the condition.
Many women report:
● Burning or stinging sensations
● Sensitivity to light
● Redness or blurred vision
● Difficulty wearing contact lenses
● A sensation of something in the eye
● Excessive tearing (a paradoxical sign of dryness)
Makeup, screen use, and eyelash enhancements like falsies or extensions can worsen symptoms, especially if lid hygiene is neglected. The good news is that practical, science-based steps can make a big difference.
What You Can Do: Simple Solutions That Work
Dry eye management is about supporting tear production, reducing inflammation, and keeping the eyelid margins healthy. Here are key tips I share with my patients:
1. Make Daily Eyelid Care a Habit
Clean your eyelid margins each day using a gentle lid cleanser or a hypochlorous acid spray. This helps clear away bacteria, debris, and leftover makeup. Avoid applying eyeliner to your waterline, as it can block the oil glands that keep your eyes comfortable. For extra precision, use a clean spoolie brush to gently sweep along the lash line and keep those glands open and healthy.
2. Use Warm Compresses
Applying heat to the eyelids helps melt and express the oils that keep the tear film stable. Microwaveable masks are convenient and effective—use them for 10 minutes daily.
3. Take Omega-3s
Clinical studies support the use of omega-3 supplements (especially from fish oil) to reduce inflammation and improve tear quality. Look for 1,000–2,000 mg per day of combined EPA and DHA in a high-quality formulation.
4. Choose the Right Artificial Tears & Ointments
Not all eye drops are created equal. Preservative-free lubricants are best for frequent use. Drops that support the oily (lipid) layer of the tear film may provide longer-lasting relief.
5. Support Eye Health
with Smart Screen Habits, Hydration, and Rest Staring at screens for extended periods can reduce your blink rate by up to 60%, contributing to eye dryness. Follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds. Stay well-hydrated by drinking at least 64 ounces of water daily. Prioritize quality sleep—it’s essential for your body’s natural healing processes, including repairing micro-damage to the ocular surface caused by dry eye.
When to See a Dry Eye Specialist
If your dry eye symptoms are ongoing or interfering with your daily life—whether it’s reading, driving, wearing makeup, or using screens—it’s time to get evaluated by an eye care professional.
Optometrists with expertise in dry eye can assess your tear quality, eyelid health, and meibomian gland function, then build a customized treatment plan. If at-home care isn’t providing enough relief, advanced options like prescription medications, in-office thermal or light-based therapies, punctal plugs, or biologic healing membranes may be recommended.
Don’t Ignore the Signs
It’s easy to dismiss dry eye as a minor annoyance, but left untreated, it can become chronic and even damage the eye’s surface. You don’t have to live with gritty, watery, or burning eyes—especially when so many effective treatments are available.
Like every other aspect of menopause, the more we understand what’s happening in our bodies, the better we can care for ourselves. Your eyes deserve attention too.
About the Author
Dr. Cheryl Chapman is an optometrist and dry eye specialist with a focus on hormonal impacts on ocular health. She is the co-founder of Peeq Pro, a luxury skincare and eyelid hygiene brand. Learn more at peeqpro.com.
The views expressed herein this article, written by a guest contributor, do not necessarily represent those of the Red Hot Mamas organization. The content is for informational purposes and should not substitute the advice of your doctor.
 Red Hot Mamas In Charge of Change.
Red Hot Mamas In Charge of Change.