By: Red Hot Mamas
Published: December 28, 2014
Diabetes Impacts you During Menopause also…
Statistics About Diabetes in the United States, based upon research from the American Diabetes Association:
- Diabetes is the 7th leading cause of death in the US
- Diabetes is a major cause of heart disease and stroke
- Diabetes is the leading cause of kidney failure, non-traumatic lower-limb amputations, and new cases of blindness among adults in the US
| Total Prevalence of Diabetes: | 25.8 million people – 8.3% of the U.S. population have diabetes |
| Diagnosed: | 18.8 million people |
| Undiagnosed: | 7.0 million people |
| Prediabetes: | 79 million people* |
| New Cases: | 1.9 million new cases of diabetes are diagnosed in people aged 20 years and older in 2010. |
| Women: | 12.6 million, or 10.8% of all women aged 20 years or older have diabetes |
* In contrast to the 2007 National Diabetes Fact Sheet, which used fasting glucose data to estimate undiagnosed diabetes and prediabetes, the 2011 National Diabetes Fact Sheet uses both fasting glucose and A1C levels to derive estimates for undiagnosed diabetes and prediabetes. These tests were chosen because they are most frequently used in clinical practice.
See more at: http://www.diabetes.org/diabetes-basics/statistics/#sthash.cly6TB6b.dpuf
See more at: http://www.diabetes.org/diabetes-basics/statistics/#sthash.2e6yDgP4.dpuf
Fast Facts on Women and Diabetes
- 12.6 million, or 10.8% of all women aged 20 years or older have diabetes
- Some women get diabetes when they are pregnant
- Women who have diabetes are more likely to have a miscarriage or a baby with birth defects
- Menopause affects diabetes because the changes in hormonal levels and balance, may lead to BG levels that are out of control. Women with diabetes are also at risk of developing premature menopause and consequent increased risks of cardiovascular disease
What is Diabetes?
Diabetes is a disease that changes the way your body uses sugar.
Some of the food you eat turns to sugar. The sugar then travels through the blood to all parts of the body. Usually, insulin helps get sugar from the blood to the body’s cells, where it is used for energy.
When you have diabetes, your body has trouble making and/or responding to insulin. So your body does not get the fuel it needs, and your blood sugar stays too high.
The Long-Term Risks of Diabetes
Undiagnosed or uncontrolled diabetes may directly cause:
- Eye retinal damage causing loss of vision
- Kidney damage
- Nerve damage causing loss of sensation or increased pain and slow digestion
- Can promote high blood pressure
- Elevation of cholesterol and triglycerides which may increase risk of heart attack
- Reduced circulation in limbs, ulcers, poor healing and limb loss
- Stroke;
- High-risk pregnancy
Diabetics must have these regular checks to avoid complications:
- Blood sugar level checks
- Cholesterol level checks
- Blood pressure checks
- Annual retina examination
- Kidney function tests
- Foot examination
What Are the Types of Diabetes?
There are two types of Diabetes.
Type 1 Diabetes is usually diagnosed in children and young adults, and was previously known as juvenile diabetes. Only 5% of people with diabetes have this form of the disease.
In type 1 diabetes, the body does not produce insulin. Insulin is the hormone that is needed to convert sugar, starches and other food into energy needed for daily life. With the help of insulin therapy and other treatments, even young children can learn to manage their condition and live long, healthy lives*
*See more at: http://www.diabetes.org/diabetes-basics/type-1/#sthash.0kbBtQAX.dpuf
Type 2 Diabetes is a problem with your body that causes blood glucose (sugar) levels to rise higher than normal. This is also called hyperglycemia.
Type 2 Diabetes is the most common form of diabetes.
If you have type 2 Diabetes your body does not use insulin properly. This is called insulin resistance. At first, your pancreas makes extra insulin to make up for it. But, over time it isn’t able to keep up and can’t make enough insulin to keep your blood glucose at normal levels*
*See more at: http://www.diabetes.org/diabetes-basics/type-2/#sthash.289iIbTO.dpuf
Are You At Risk for Type 1 Diabetes?
There aren’t many known risk factors for type 1 diabetes, but some known risk factors include:
- A family history. Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing the condition.
- Genetics. The presence of certain genes indicates an increased risk of developing type 1 diabetes. In some cases — usually through a clinical trial — genetic testing can be done to determine if someone who has a family history of type 1 diabetes is at increased risk of developing the condition.
- Geography. The incidence of type 1 diabetes tends to increase as you travel away from the equator. People living in Finland and Sardinia have the highest incidence of type 1 diabetes — about two to three times higher than rates in the United States and 400 times that of people living in Venezuela.
Possible risk factors for type 1 diabetes include:
- Viral exposure. Exposure to Epstein-Barr virus, coxsackievirus, mumps virus or cytomegalovirus may trigger the autoimmune destruction of the islet cells, or the virus may directly infect the islet cells.
- Early vitamin D. Research suggests that vitamin D may be protective against type 1 diabetes. However, early drinking of cow’s milk — a common source of vitamin D — has been linked to an increased risk of type 1 diabetes.
- Other dietary factors. Omega-3 fatty acids may offer some protection against type 1 diabetes. Drinking water that contains nitrates may increase the risk. Consuming dairy products, particularly cow’s milk, may increase infants’ risk of the disease. Additionally, the timing of the introduction of cereal into a baby’s diet may affect risk. One clinical trial found that between ages 3 and 7 months appears to be the optimal time for introducing cereal.
- Some other possible risk factors include:
- Having a mother younger than age 25 when she gave birth to you.
- Having a mother who had preeclampsia during pregnancy.
- Being born with jaundice.
- Having a respiratory infection just after birth.
Symptoms of Type 1 Diabetes
Common Symptoms:
- Increased thirst
- Passing water very frequently
- Tiredness and lack of energy
- Blurry vision
- Weight loss – even though you are eating more
- Poor concentration and sometimes collapse
(See your doctor if you have any of these symptoms)
Are You At Risk For Type 2 Diabetes?
Researchers don’t fully understand why some people develop type 2 diabetes and others don’t. It’s clear, however, that certain factors increase the risk, including:
- Weight. Being overweight is a primary risk factor for type 2 diabetes. The more fatty tissue you have, the more resistant your cells become to insulin.
- Fat distribution. If your body stores fat primarily in your abdomen, your risk of type 2 diabetes is greater than if your body stores fat elsewhere, such as your hips and thighs.
- Inactivity. The less active you are, the greater your risk of type 2 diabetes. Physical activity helps you control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent or sibling has type 2 diabetes.
- Race. Although it’s unclear why, people of certain races — including blacks, Hispanics, American Indians and Asian-Americans — are more likely to develop type 2 diabetes than whites are.
- Age. The risk of type 2 diabetes increases as you get older, especially after age 45. That’s probably because people tend to exercise less, lose muscle mass and gain weight as they age. But type 2 diabetes is also increasing dramatically among children, adolescents and younger adults because they are overweight.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Gestational diabetes. If you developed gestational diabetes when you were pregnant, your risk of later developing type 2 diabetes increases. If you gave birth to a baby weighing more than 9 pounds (4 kilograms), you’re also at risk of type 2 diabetes.
Women and Type 2 Diabetes Risk Factors
- Women with high risk factor for type 2 diabetes have a greater risk for developing cardiovascular disease (CVD), and the risk increases with age.
- A postmenopausal woman who has type 2 diabetes is 3 times more likely to develop CVD or stroke and is 4 times more likely to die from a myocardial infarction than a woman without the disease.
- Women with type 2 diabetes are at increased risk for developing endometrial cancer, colorectal cancer, and a risk of gallstones is doubled. In uncontrolled type 2 diabetes, some women may experience complications that include neuropathy, renal failure, vision loss, or amputation.
Symptoms of Type 2 Diabetes
The following symptoms of diabetes are typical. However, some people with type 2 Diabetes have symptoms so mild that they go unnoticed.
Symptoms include:
- Needing to pass urine often (including needing to get up at night)
- Constant thirst
- Feeling very hungry – even though you are eating
- Recurrent yeast infections, boils or minor skin infections
- Cuts and bruises that are slow to heal
- Feeling generally tired, extremely fatigued, and run down
- Blurry vision
- Tingling, pain, or numbness in the hands/feet
(See your doctor if you have any of these symptoms)
How Does Someone Know if He/She Has Diabetes?
Diagnosing diabetes at an early stage is crucial if you want to avoid the serious complications it causes.
Tests to Diagnose Diabetes
- Type 1 diabetes testing include the: Glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. It works by measuring the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates you have diabetes.
- There are two different tests your doctor can use for Type 1 and Type 2 diabetes used to measure your blood glucose to determine if you have pre-diabetes or diabetes:
- The fasting plasma glucose test (FPG) or the oral glucose tolerance test (OGTT). In general, it is recommended that any blood test that is outside the normal range be repeated on a different day to confirm the diagnosis. The American Diabetes Association recommends the FPG because it is easier, faster, and less expensive to perform.
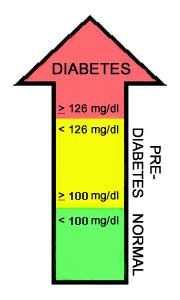
- The FPG test is a blood test that determines the amount of glucose (sugar) in the blood after an overnight fast (not eating for at least 8 hours). A fasting blood glucose level between 100 and 125 mg/dl means a person has pre-diabetes. A fasting blood glucose level of 126 mg/dl or higher means a person has diabetes.
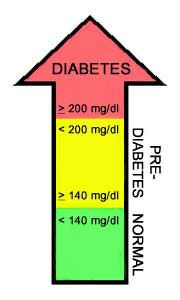
- With the OGTT test, a person’s blood glucose level is measured after fasting and then 2 hours after drinking a glucose-rich beverage. If the 2-hour blood glucose level is between 140 and 199 mg/dl, the person has pre-diabetes. If the 2-hour blood glucose level is at 200 mg/dl or higher, the person has diabetes.
See the chart below for the ranges of blood sugar levels and how they are used to diagnose pre-diabetes and diabetes.
| Diagnosing Pre-Diabetes and Diabetes | |
 |
 |
|
Fasting Plasma Glucose |
Oral Glucose Tolerance Test |
If you’re diagnosed with diabetes, your doctor will also run blood tests to check for autoantibodies that are common in type 1 diabetes.
These tests help your doctor distinguish between type 1 and type 2 diabetes. The presence of ketones — byproducts from the breakdown of fat — in your urine also suggests type 1 diabetes, rather than type 2.
How is Diabetes Managed?
Diabetes is managed by keeping blood sugar under control and as close to normal as possible.. This is the key to avoiding complications and discomfort. Here are some ways to manage diabetes:
Exercise. 30 minutes a day, most days of the week.
Regular physical activity helps to manage diabetes because active muscles use glucose without the need of insulin!. You should talk to your doctor or health care provider before starting any exercise plan. Some good ways to get exercise are to:
- Take a brisk walk (outside or inside on a treadmill).
- Go dancing.
- Take a low-impact aerobics class.
- Swim or do water aerobic exercises.
- Play tennis.
- Ride a stationary bicycle indoors.
Here are some ideas for being more active everyday:
- Park the car farther away from your destination.
- Take the stairs instead of the elevator or escalator.
- Exercise while watching TV.
- Take the dog for a walk.
- Work in the garden.
- Clean the house.
- At work, walk over to see a co-worker instead of calling or emailing.
- During your lunch break, walk to do your errands.
Choose Healthy Food
Good nutrition is a very important part of diabetes management. People with diabetes should work with their diabetes healthcare team to develop an eating plan that meets their personal food preferences while keeping blood glucose in a healthy range.
Choose nutritious foods and get plenty of physical activity level. By doing this, blood sugar levels can be kept as close to normal as possible.
Here are some helpful tips on making healthy food choices:
- Eat lots of vegetables and fruits. Try picking from the rainbow of colors available to add variety to your meals.
- Choose whole grain foods instead of processed grain products like white bread, white rice or regular pasta. Try brown rice with your stir-fry or whole wheat spaghetti with your favorite pasta sauce.
- Include fish in your meals two to three times a week.
- Choose lean meats like chicken and turkey without the skin. To prepare meats and fish with less fat, trim any visible fat and use low-fat cooking methods such as broiling, grilling, roasting, poaching or stir-frying.
- Include dried beans (like kidney or pinto beans) and lentils in your meals.
- Choose low fat dairy products such as milk, yogurt and cheese (1 percent fat or less).
- Choose liquid oils such as canola, olive or peanut oil for cooking, instead of solid fats such as butter, lard and shortening. Remember that all fats are high in calories. Choose fruit that is in-season for dessert – you’ll get more flavor and pay less too! Try to cut back on high-calorie dessert and snack foods such as chips, cookies, cakes and ice cream that give you and your family little nutrition.
- Choose water and calorie-free “diet” drinks instead of regular soda, fruit punch, sweet tea and other sugar-sweetened drinks.
- Decrease the amount of sugar (if possible stop) adding it to your coffee, teas, etc.
- Control your portion sizes.
How Can You Help Yourself?
Medication
People with type 1 diabetes must use insulin. Some people with type 2 diabetes can manage their diabetes with healthy eating and exercise. However, your doctor may need to also prescribe oral medications (pills) and/or insulin to help you meet your target blood glucose levels.
Insulin and Other Injectables
Insulin is a naturally occurring hormone secreted by the pancreas. Many people with diabetes are prescribed insulin, either because their bodies do not produce insulin (type 1 diabetes) or do not use insulin properly (type 2 diabetes).
There are more than 20 types of insulin sold in the United States. These insulin’s differ in how they are made, how they work in the body, and how much they cost. You should discuss with your doctor to gain an understanding of what the right type of insulin he/she recommends for your health.
When the body cannot make enough insulin, you can take insulin by injection or through use of an insulin pump, depending on how quickly they work, when they peak, and how long they last. Insulin is available in different strengths; the most common is U-100.
Fine-Tuning Your Blood Glucose
Many factors affect your blood glucose levels, including the following:
- What you eat
- How much and when you exercise
- Where you inject your insulin
- When you take your insulin injections
- Illness
- Stress
Oral Medications What Are My Options?
Many options are available and your clinician can choose amongst them. Be it with insulin, or with oral medication, if they decrease the serum level of glucose too much it may cause symptoms of hypoglycemia. Some of these symptoms may be confounded with the symptoms of menopause (nervousness, palpitations, sweating, irritability, to name a few).
Resources:
The American Diabetes Association www.diabetes.org
American Association of Clinical Endocrinologists (AACE) www.aace.com
The Endocrine Society www.endocrine.org
Hormone Health Network www.hormone.org
Center for Disease Control and Prevention (CDC) www.cdc.gov/diabetes
 Red Hot Mamas In Charge of Change.
Red Hot Mamas In Charge of Change.


